Table of Contents
| Introduction | Sexual Maturity |
| Female Reproductive System | Male Reproductive System |
| Fertilization |
Introduction
The Aging Male Reproductive System fertility and sexual function decline with age Human Anatomy & Physiology: Reproductive System; Ziser Lecture Notes, 2013.4 19! Due to declining levels of sex hormones age 50 men go through a period of physical and psychological change = climacteric in males, testosterone secretion peaks at 20 then. The female reproductive system has two functions: The first is to produce egg cells, and the second is to protect and nourish the offspring until birth. The uterus is a muscular pear-shaped structure where a fetus will develop during pregnancy. ASSUME A COUPLE HAS JUST CONSUMMATED THE SEX ACT AND THE SPERM HAVE BEEN DEPOSITED IN THE VAGINA. TRACE THE PATHWAY OF THE SPERM THROUGH THE FEMALE REPRODUCTIVE TRACT. VAGINA - CERVIX - UTERUS - UTERINE TUBE - PERITONEAL CAVITY. The reproduction system in males the penis, scrotum, testicles (testes), Vas deferens, seminal vesicles, prostate gland, and the urethra. Drugs, environmental factors, genetics, age, and disease can affect how these structures function, for example, sexual function and libido, enlarged prostate, urinary tract infections, and prostate cancer.
Effective public health programs, research, and policy relating to human sexuality, pregnancy, contraception, and the transmission of sexually transmitted infections (including HIV) depends upon knowledge of the structure (anatomy) and function (physiology) of the male and female reproductive systems.
Sexual and Reproductive Development
Human beings are sexual throughout life. Sexuality encompasses more than sexual behavior - it is not only the physical, but the mental and spiritual as well. Sexuality is a core component of personality and a fundamental part of human life. While the problems usually associated with sexual behavior are real and need to be addressed, human sexuality also has significant meaning and value in each individual's life.
Reproductive Biology
Reproductive physical maturity and the capacity for human reproduction begin during puberty, a period of rapid growth and change experienced by both males and females. Puberty is not an isolated event, but a process which takes place over several years.

During puberty, the hypothalamus (a gland located at the base of the brain which regulates temperature, sleep, emotions, sexual function and behavior) produces hormones (chemicals that originate in a gland or organ and travel through the blood to another organ, stimulating it by chemical action to increase functional activity and secretions).
These hormones stimulate the gonads, the reproductive glands (the testes in males and the ovaries in females) to produce testosterone (males) and estrogen and progesterone (females).
Male puberty generally occurs between the ages of 13-15 and is characterized by the secretion of the male hormone testosterone, which stimulates spermatogenesis (sperm production), and the development of secondary sexual characteristics (increased height and weight, broadening shoulders, growth of the testes and penis, pubic and facial hair growth, voice deepening, and muscle development).
Female puberty generally occurs between the ages of 9-13, and results in ovulation and menstruation, which involve cyclic hormonal changes in estrogen and progesterone. Secondary sexual characteristics (growth of pubic and underarm hair, breast enlargement, vaginal and uterine growth, widening hips, increased height, weight and fat distribution) also occur as part of the female pubertal process.
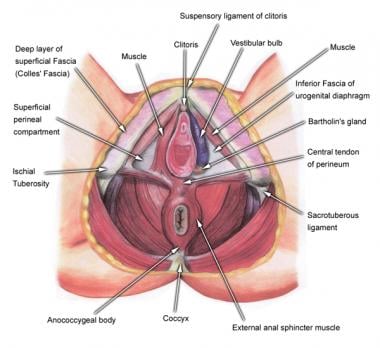
Female Reproductive System
Understanding female reproductive anatomy includes the study of the external and internal structures; and the hormonal cycle.
Structures
The external genitalia, also called the vulva, includes the mons pubis (a fatty mound which covers the pubic bone), the labia majora (outer lips of the vagina), the labia minora (the inner lips of the vagina), the vaginal opening, the urethral opening (opening of the urethra, a tube which carries urine from the bladder outside of the body), the clitoris (a small structure with sensitive nerve endings located within the labia minora, the sole purpose of which is for sexual arousal and pleasure), and the perineum (the space between the anus (the rectal opening), and the vaginal opening).
The internal reproductive anatomy includes the uterus, two ovaries, two fallopian tubes, the urethra, the pubic bone, and the rectum. The uterus contains an inner lining called the endometrium (which builds ups and sheds monthly in response to hormonal stimulation). The lower portion of the uterus is called the cervix, which contains a small opening called the os. Menstrual blood flows through the os into the vagina during menstruation. Semen travels through the os into the uterus and the fallopian tubes following ejaculation during sexual intercourse. The cervical os dilates (opens) during childbirth.
The ovaries, two small almond-shaped structures located on each side of the uterus, are the female gonads (reproductive glands). Female babies are born with over 400,000 ova (the gametes, also referred to as egg cells or oocytes), which are stored in the ovaries. The female body does not produce any additional ova. The ovaries produce estrogen and progesterone. The ovaries are close to, but not actually connected to the fallopian tubes, thin tube-like structures that are the site of fertilization, the fusion of the male and female gametes.
The Menstrual/Hormonal Cycle
The hormonal cycle facilitates maturation and rupture of the ovarian follicle resulting in the release of an ovum (the female reproductive or germ cell). Each month a series of changes take place which prepares the uterus for pregnancy. This cycle (menstrual cycle) is described below:
The first day of menstruation (referred to as Day 1) occurs when levels of estrogen and progesterone are low. In response to these low levels, the hypothalamus secretes gonadotrophin releasing hormone (GnRH) which triggers the anterior pituitary gland to release two hormones: follicle stimulating hormone (FSH), and luteinizing hormone (LH).
FSH stimulates the development of many follicles within the ovary. One dominant follicle takes over. As it continues to grow, it produces increasing amounts of estrogen, which stimulates the release of LH, and inhibits FSH, which suppresses further follicular development.
When LH levels are highest (LH surge), the ovarian follicle ruptures and releases one ovum, which is swept into the fallopian tube by hair-like projections called cilia that line the fimbriae (the fringe-like end of the fallopian tube that is closest to the ovary). This process is called ovulation. Increasing estrogen levels causes the cervical mucous (vaginal secretions) to become clear and profuse and the os to dilate. These two actions may facilitate the transport of semen (containing sperm) from the vagina, through the uterus, and into the fallopian tube.
Following ovulation, the ruptured follicle is transformed into the corpus luteum, a glandular mass that continues to produce estrogen and high levels of progesterone. The progesterone causes the endometrium to thicken, preparing it for implantation of a fertilized egg. If fertilization takes place during ovulation, hormonal levels remain high, essential for the maintenance of the pregnancy.
If fertilization does not occur, the corpus luteum shrinks and levels of both estrogen and progesterone decrease. The withdrawal of estrogen and progesterone cause the blood vessels of the endometrial (uterine) lining to break resulting in vaginal bleeding (menstruation). The average menstrual cycle is 28-35 days, and menstrual flow usually continues for three to seven days, although there are variations among women.
Following menstruation, estrogen and progesterone levels are low, triggering the hypothalamus to once again release GnRH, starting the entire cycle again. If fertilization does take place, menstruation will not reoccur for the duration of the pregnancy
Menopause

Menopause, the end of menstruation, occurs between the ages of 45 and 55 (with the average age of 51.3). An entirely normal developmental and physiological process, it can be accompanied by symptoms including hot flashes, fatigue, moodiness, insomnia, decreased libido and sexual response, changes in memory, weight gain, and vaginal dryness. Until cessation of ovarian function is confirmed through a blood test, and/or one year of no menses, women may continue to ovulate and therefore require contraception to prevent unintended pregnancy.
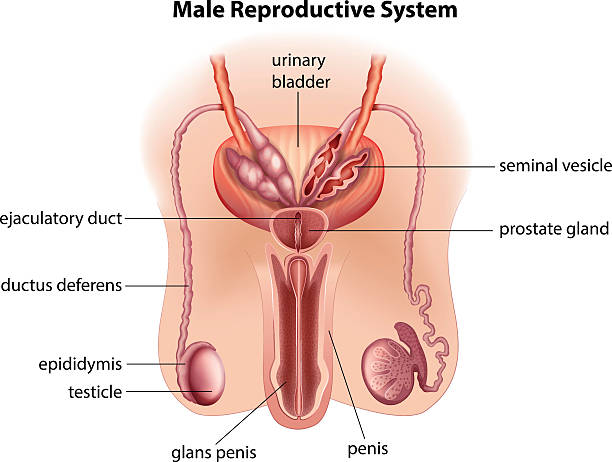
Male Reproductive System
To understand the male reproductive system, one must know the external and internal structures, and the process of spermatogenesis (sperm production) including the physiologic pathway of the sperm cell.
Structures
The male external structures are the penis and the scrotum (a pouch which protects the testes). The penis consists of the glans (the head), and the shaft (the body). The glans is covered by a fold of skin called the foreskin (circumcision removes the foreskin). The scrotum surrounds and protects the two testes, internal structures also referred to as testicles.
The testes are the male gonads and contain hundreds of tiny seminiferous tubules where sperm cells are produced. The epididymis is a small oblong body which rests on the surface of the testes where sperm mature and are stored. The epididymis leads into the vas deferens (narrow tubes which carry sperm away from the testes). The vas deferens extends to join with the ducts of the two seminal vesicles (located on side of the prostate gland) to form the ejaculatory ducts which extend through the body of the prostate gland and empty into the urethra. The prostate gland surrounds the neck of the bladder (the structure that stores urine) and the urethra, (a thin tube which extends through the penis and carries semen and urine outside of the body, although not simultaneously). The Cowper's glands (also called the bulbourethral glands) are found on each side of the urethra, just below the prostate gland.
Process of Spermatogenesis
Spermatogenesis begins in the seminiferous tubules of the testes. Sperm pass into the epididymis where they mature and become motile so they are able to move through the vas deferens and into the seminal vesicles where they mix with seminal fluids, rich in fructose and other nutrients. The prostate gland and the Cowper's glands secrete fluids which also help to nourish and transport the sperm. This mixture of fluids and sperm is called semen, the fluid which is expelled from a man's penis during ejaculation. Sexual arousal can cause fluid from the Cowper's glands to be released prior to ejaculation. This fluid is called pre-ejaculatory fluid and does not contain sperm unless it is leftover from a previous ejaculation. Contrary to popular belief, there is little evidence to support that pre-ejaculatory fluid contains enough sperm to cause pregnancy.
Although men continue to produce sperm throughout their lives, testosterone production decreases at about 45-65 years of age.
Fertilization
During coitus (sexual intercourse) between a male and a female, semen is released into the vagina and transported through the uterus into the fallopian tube. Although many factors contribute to whether or not a single act of intercourse will result in pregnancy, most important is whether or not a sperm cell will meet an ovum in the fallopian tube (fertilization). Fertilization can only occur if intercourse takes place before the time of ovulation that usually occurs mid-cycle, or about 14 days before the woman's next menstrual period. At the time of ovulation, the ovum is released from the ovary and transported in the fallopian tube where it remains for about 24-48 hours. Pregnancy is most likely to occur if fresh semen is present when ovulation occurs.
Sperm cells remain viable within the female reproductive tract for about 72 hours. Only a single sperm cell is needed to fertilize the ovum, even though the average ejaculation contains approximately 300 million sperm.
During fertilization, the sperm enters the cell membrane of the ovum so the nuclei of the sperm and egg cells combine to form a zygote. The zygote will remain in the fallopian tube for approximately three days before it travels to the uterus where it will remain for approximately four to five days before implantation into the uterine lining.
Ectopic Pregnancy
An ectopic pregnancy is when a fertilized egg becomes implanted outside the uterus, most often in the fallopian tubes. Ectopic pregnancies are often the result of fallopian tube scarring caused by untreated sexually transmitted infections, which impedes the transport of the zygote from the fallopian tubes to the uterus. If left undiagnosed or untreated, the zygote grows in the fallopian tube, and may result in fallopian rupture. Without medical or surgical intervention, ectopic pregnancy usually results in infertility, severe infection, or death. Ectopic pregnancy can be difficult to diagnose, as it shares many symptoms with uterine pregnancy. However, Some symptoms of ectopic pregnancy include pain in the vagina, abdomen, or lower back, vaginal bleeding or spotting, dizziness, fainting, and low blood pressure.
Sex Determination
Prior to fertilization, the sperm and egg cells have only half the number of chromosomes (the genetic determinants of heredity) of other body cells because they go through a process of cell division called meiosis, which reduces the number of chromosomes from 46 to 23. The 23 chromosomes from the sperm cell combine with the 23 chromosomes from the ovum to form a single cell (zygote) consisting of 46 chromosomes.
Anatomy Reproductive System Exam
Sex of the offspring is determined by whether the sperm contains an X or a Y sex chromosome. Female ova always carry an X chromosome. If the sperm cell contains a Y chromosome, the offspring will be a male (XY pair). If it contains an X chromosome, the offspring will be a female (XX pair). Thus, the sperm biologically determines sex.
In this image, you may find a Male Genital System Diagram.
We are pleased to provide you with the picture named Male Genital System Diagram. We hope this picture Male Genital System Diagram can help you study and research. for more anatomy content please follow us and visit our website: www.anatomynote.com.
Anatomynote.com found Male Genital System Diagram from plenty of anatomical pictures on the internet. We think this is the most useful anatomy picture that you need. You can click the image to magnify if you cannot see clearly.
This image added by admin. Thank you for visit anatomynote.com. We hope you can get the exact information you are looking for. Please do not forget to share this page and follow our social media to help further develop our website. If you have any question please do not hesitate to contact us.
If you think this picture helpful, please don't forget to rate us below the picture!
One of our purpose to collect these pictures is we hope these pictures will not be lost when the relevant web page is deleted.
But you may also know any content, trademark/s, or other material that might be found on the anatomynote.com website that is not anatomynote.com property remains the copyright of its respective owner/s. In no way does anatomynote.com claim ownership or responsibility for such items, and you should seek legal consent for any use of such materials from its owner.
Anatomy Reproductive System Female
Anatomy is the amazing science. It can help you understand our world more detailed and specific. We hope you will use this picture in the study and helping your research.